Is strep throat a localized infection, or can it spread? Yes, strep throat, while typically affecting the throat and tonsils, can indeed travel to other parts of the body if left untreated, potentially leading to serious complications. At familycircletravel.net, we aim to keep your family healthy and informed during your travels, preventing health issues before they arise and keeping your family trip memorable. Keep reading to learn about causes and ways to prevent.
1. What Exactly is Strep Throat?
Strep throat is a bacterial infection caused by the Group A Streptococcus bacteria. It primarily affects the throat and tonsils, causing inflammation and discomfort. This infection is highly contagious and commonly spreads through close contact with infected individuals.
1.1. How Common is Strep Throat?
Strep throat is more prevalent in children between 5 and 15 years old, but it can affect individuals of any age. According to the Centers for Disease Control and Prevention (CDC), strep throat accounts for a significant percentage of sore throat cases, particularly during the school year.
1.2. What are the Initial Symptoms of Strep Throat?
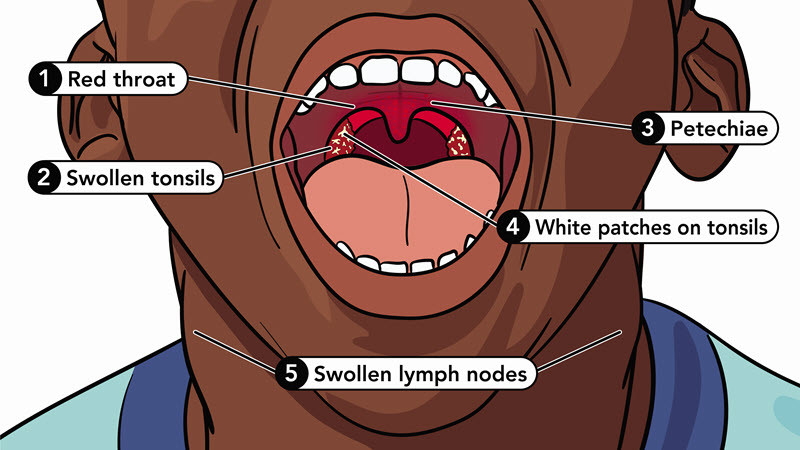
The initial symptoms of strep throat typically appear 2 to 5 days after exposure to the bacteria. Common symptoms include:
- A sore throat that starts quickly
- Pain when swallowing
- Red and swollen tonsils, sometimes with white patches or streaks of pus
- Fever
- Swollen lymph nodes in the front of the neck
- Tiny, red spots on the roof of the mouth (petechiae)
If your family experiences these symptoms, it is important to seek medical attention promptly to prevent further complications.
2. How Does Strep Throat Spread?
Understanding how strep throat spreads is crucial for prevention, especially when traveling with family. The bacteria that causes strep throat is highly contagious and primarily spreads through respiratory droplets.
2.1. What are the Common Modes of Transmission?
The most common ways strep throat spreads include:
- Close Contact: Direct contact with an infected person, such as kissing or sharing utensils.
- Respiratory Droplets: Coughing or sneezing releases droplets containing the bacteria into the air, which can be inhaled by others.
- Contaminated Surfaces: Touching surfaces with the bacteria and then touching the face, particularly the mouth or nose.
2.2. How Can You Prevent the Spread of Strep Throat?
Preventing the spread of strep throat involves several key measures:
- Frequent Handwashing: Wash hands thoroughly with soap and water for at least 20 seconds, especially after coughing, sneezing, or being in public places.
- Avoid Sharing: Do not share utensils, cups, or personal items with others.
- Cover Mouth and Nose: When coughing or sneezing, cover the mouth and nose with a tissue or the elbow.
- Use Hand Sanitizer: Carry and use hand sanitizer with at least 60% alcohol when soap and water are not available.
These preventive measures are essential for maintaining your family’s health during travels, minimizing the risk of contracting and spreading strep throat.
3. Can Strep Throat Travel to Other Parts of the Body?
While strep throat primarily affects the throat and tonsils, the infection can spread to other parts of the body if left untreated. Understanding how this spread occurs and the potential complications is vital for ensuring timely and effective medical care.
3.1. How Does the Bacteria Spread Beyond the Throat?
If strep throat is not treated with antibiotics, the bacteria can spread from the throat to other areas, leading to various complications:
- Direct Extension: The infection can directly extend to nearby tissues, such as the sinuses or ears.
- Bloodstream: In rare cases, the bacteria can enter the bloodstream, leading to more widespread infections.
- Immune Response: Some complications arise from the body’s immune response to the strep bacteria, affecting organs like the kidneys and heart.
3.2. What are the Potential Complications of Untreated Strep Throat?
Untreated strep throat can lead to several serious complications:
- Rheumatic Fever: This is a serious inflammatory condition that can affect the heart, joints, brain, and skin. It can lead to permanent heart damage known as rheumatic heart disease.
- Post-Streptococcal Glomerulonephritis: This kidney disease occurs when the immune system’s response to the strep infection damages the kidneys.
- Peritonsillar Abscess: This is a collection of pus behind the tonsils, causing severe pain and difficulty swallowing.
- Ear Infections: The infection can spread to the middle ear, causing otitis media.
- Sinus Infections: Strep bacteria can also spread to the sinuses, leading to sinusitis.
- Scarlet Fever: Characterized by a distinctive rash that starts on the neck and chest and spreads throughout the body.
 Child experiencing strep throat symptoms
Child experiencing strep throat symptoms
Recognizing symptoms early can reduce the chance of complications for children with strep throat.
These complications highlight the importance of early diagnosis and treatment of strep throat, particularly for families traveling where access to immediate medical care may be limited.
4. Rheumatic Fever: A Serious Complication of Strep Throat
Rheumatic fever is one of the most severe complications of untreated or poorly managed strep throat. This inflammatory disease can have long-lasting effects on various parts of the body.
4.1. What is Rheumatic Fever and How Does it Develop?
Rheumatic fever is an inflammatory disease that can develop after a strep throat infection. It is caused by the body’s immune response to the strep bacteria, which can mistakenly attack the body’s own tissues.
4.2. What are the Symptoms of Rheumatic Fever?
The symptoms of rheumatic fever typically appear 1 to 5 weeks after a strep throat infection. These symptoms can vary but often include:
- Fever: Elevated body temperature.
- Joint Pain: Pain and inflammation in the joints, particularly the knees, ankles, elbows, and wrists. The pain may migrate from one joint to another.
- Carditis: Inflammation of the heart, which can lead to shortness of breath, chest pain, and heart murmurs.
- Sydenham’s Chorea: Involuntary movements of the hands, feet, and face.
- Erythema Marginatum: A distinctive, painless rash with clear edges that appears on the trunk and limbs.
- Subcutaneous Nodules: Small, painless lumps under the skin, usually near the joints.
4.3. How Does Rheumatic Fever Affect the Heart?
Rheumatic fever can cause significant damage to the heart, leading to rheumatic heart disease. The inflammation can affect the heart valves, causing them to become scarred and narrowed or leaky. This damage can lead to:
- Heart Murmurs: Abnormal heart sounds caused by turbulent blood flow through the damaged valves.
- Shortness of Breath: Difficulty breathing, especially during physical activity.
- Chest Pain: Discomfort or pain in the chest.
- Heart Failure: The heart’s inability to pump enough blood to meet the body’s needs.
Rheumatic heart disease is a chronic condition that can require lifelong medical management, including medications and, in some cases, surgery.
4.4. What is the Long-Term Outlook for Individuals with Rheumatic Heart Disease?
The long-term outlook for individuals with rheumatic heart disease depends on the severity of the heart damage and the effectiveness of ongoing medical care. Some individuals may experience mild symptoms and require only regular monitoring, while others may face more severe complications and require extensive treatment.
Effective management of rheumatic heart disease includes:
- Antibiotics: To prevent recurrent strep infections and further damage to the heart.
- Medications: To manage symptoms such as heart failure and arrhythmias.
- Surgery: In severe cases, valve repair or replacement may be necessary.
For families planning trips, especially to remote areas, understanding the risks and preventive measures associated with rheumatic fever is crucial for ensuring the health and safety of their children.
5. Post-Streptococcal Glomerulonephritis: Kidney Complications from Strep
Post-streptococcal glomerulonephritis (PSGN) is another serious complication that can arise from a strep throat infection, affecting kidney function.
5.1. What is Post-Streptococcal Glomerulonephritis?
PSGN is a kidney disease that develops after a strep throat infection. It occurs when the immune system’s response to the strep bacteria damages the glomeruli, which are the filtering units of the kidneys.
5.2. What are the Symptoms of Post-Streptococcal Glomerulonephritis?
The symptoms of PSGN typically appear 1 to 3 weeks after a strep throat infection. These symptoms can include:
- Hematuria: Blood in the urine, causing it to appear pink or cola-colored.
- Edema: Swelling in the face, hands, and feet.
- Hypertension: High blood pressure.
- Decreased Urination: Reduced urine output.
- Fatigue: Feeling tired and weak.
5.3. How Does PSGN Affect Kidney Function?
PSGN can impair the kidneys’ ability to filter waste and excess fluids from the blood. The inflammation and damage to the glomeruli can lead to:
- Proteinuria: Protein in the urine.
- Fluid Retention: Leading to edema and high blood pressure.
- Acute Kidney Injury: In severe cases, PSGN can cause a sudden loss of kidney function.
5.4. What is the Treatment and Prognosis for PSGN?
The treatment for PSGN focuses on managing the symptoms and supporting kidney function. This may include:
- Medications: To control high blood pressure and reduce swelling.
- Diuretics: To help the body eliminate excess fluid.
- Dietary Restrictions: Limiting salt and fluid intake.
- Dialysis: In severe cases, dialysis may be necessary to filter the blood.
The prognosis for PSGN is generally good, particularly in children. Most individuals recover completely within a few weeks to months. However, some may experience long-term kidney damage or develop chronic kidney disease.
Families traveling with children should be aware of the signs and symptoms of PSGN and seek prompt medical attention if they suspect their child may have developed this complication after a strep throat infection.
6. Other Localized Infections: Abscesses, Ear Infections, and Sinus Infections
Besides systemic complications like rheumatic fever and PSGN, strep throat can also lead to localized infections in nearby tissues.
6.1. Peritonsillar Abscess: What is it and How Does it Develop?
A peritonsillar abscess is a collection of pus that forms behind the tonsils. It typically develops when a strep throat infection spreads to the surrounding tissues.
6.2. What are the Symptoms of a Peritonsillar Abscess?
The symptoms of a peritonsillar abscess can include:
- Severe Sore Throat: Often on one side.
- Difficulty Swallowing: Pain when swallowing, making it hard to eat or drink.
- Fever: Elevated body temperature.
- Muffled Voice: Difficulty speaking clearly.
- Swollen Lymph Nodes: In the neck.
- Trismus: Difficulty opening the mouth.
6.3. How is a Peritonsillar Abscess Treated?
Treatment for a peritonsillar abscess typically involves:
- Drainage: Draining the pus from the abscess.
- Antibiotics: To treat the underlying infection.
- Pain Management: Medications to relieve pain and discomfort.
In some cases, a tonsillectomy (surgical removal of the tonsils) may be recommended to prevent future occurrences.
6.4. Ear Infections and Sinus Infections: How Can Strep Lead to These?
Strep bacteria can also spread to the middle ear and sinuses, leading to ear infections (otitis media) and sinus infections (sinusitis). These infections can cause:
- Ear Pain: In the case of ear infections.
- Sinus Pressure: Facial pain and congestion in the case of sinus infections.
- Fever: Elevated body temperature.
- Nasal Congestion: Runny or stuffy nose.
- Headache: Pain in the head.
6.5. What are the Treatments for Ear Infections and Sinus Infections Caused by Strep?
Treatment for ear and sinus infections caused by strep typically involves:
- Antibiotics: To eliminate the bacteria.
- Pain Relief: Medications to manage pain and fever.
- Decongestants: To relieve nasal congestion.
For families on the go, knowing the potential for these localized infections and how to address them can help ensure a smooth and healthy travel experience.
7. Risk Factors for Strep Throat and its Spread
Several risk factors can increase the likelihood of contracting strep throat and its subsequent spread. Being aware of these factors can help families take necessary precautions.
7.1. Age: Why are Children More Susceptible?
Children, particularly those between 5 and 15 years old, are more susceptible to strep throat. This is primarily due to:
- Close Contact: Children in this age group often spend time in close proximity to one another in schools and daycare centers.
- Hygiene Practices: Younger children may not have fully developed hygiene practices, increasing the risk of transmission.
- Immune System: Children’s immune systems are still developing, making them more vulnerable to infections.
7.2. Close Contact: How Does Proximity Increase Risk?
Close contact with infected individuals is a significant risk factor for strep throat. This includes:
- Household Members: Sharing a household with someone who has strep throat increases the risk of transmission.
- Classmates: Children in close contact at school are more likely to spread the infection.
- Crowded Settings: Spending time in crowded settings, such as daycare centers or public transportation, can increase exposure to the bacteria.
7.3. Weakened Immune System: Conditions that Increase Vulnerability
Individuals with weakened immune systems are more vulnerable to strep throat and its complications. Conditions that can weaken the immune system include:
- Chronic Illnesses: Such as diabetes or autoimmune disorders.
- Immunosuppressant Medications: Such as those taken after organ transplants.
- HIV/AIDS: Which weakens the immune system.
For families with members who have weakened immune systems, extra precautions are necessary to prevent strep throat and its spread.
8. Diagnosis of Strep Throat: Ensuring Accurate and Timely Detection
Accurate and timely diagnosis of strep throat is essential for preventing complications and ensuring appropriate treatment.
8.1. Rapid Strep Test: How Does it Work?
The rapid strep test is a common diagnostic tool used to detect strep throat. It involves:
- Swabbing the Throat: A healthcare provider will use a sterile swab to collect a sample from the back of the throat and tonsils.
- Testing the Sample: The swab is then tested for the presence of Group A Streptococcus bacteria.
- Results: The results are typically available within minutes.
8.2. Throat Culture: When is it Necessary?
A throat culture may be necessary if the rapid strep test is negative but strep throat is still suspected. This involves:
- Swabbing the Throat: Similar to the rapid strep test, a sample is collected from the throat.
- Culturing the Sample: The sample is then cultured in a laboratory to allow bacteria to grow.
- Results: Results usually take 24 to 48 hours.
A throat culture is more sensitive than the rapid strep test and can detect even small amounts of bacteria.
8.3. Why is Accurate Diagnosis Important?
Accurate diagnosis of strep throat is crucial for several reasons:
- Preventing Complications: Early diagnosis and treatment can prevent serious complications such as rheumatic fever and PSGN.
- Avoiding Unnecessary Antibiotics: Viral infections can cause sore throats. Antibiotics are ineffective against viruses, so accurate diagnosis helps avoid unnecessary antibiotic use.
- Reducing Spread: Prompt treatment can reduce the spread of the infection to others.
9. Treatment Options for Strep Throat: Antibiotics and Supportive Care
The primary treatment for strep throat involves antibiotics to eliminate the bacteria and supportive care to relieve symptoms.
9.1. Antibiotics: Which Medications are Commonly Prescribed?
Antibiotics are the main treatment for strep throat. Commonly prescribed medications include:
- Penicillin: This is the most common antibiotic prescribed for strep throat.
- Amoxicillin: This is another penicillin-based antibiotic that is often used, especially for children.
- Cephalexin: This is a cephalosporin antibiotic that can be used for individuals who are allergic to penicillin.
- Azithromycin: This is a macrolide antibiotic that is sometimes used for individuals who are allergic to penicillin, although resistance to this antibiotic is increasing.
9.2. How Long Does it Take for Antibiotics to Work?
Most individuals start to feel better within 24 to 48 hours after starting antibiotics. It is important to complete the entire course of antibiotics, even if symptoms improve, to ensure that the infection is completely eradicated.
9.3. What are the Potential Side Effects of Antibiotics?
Antibiotics can cause side effects, including:
- Nausea: Feeling sick to the stomach.
- Diarrhea: Loose, watery stools.
- Stomach Pain: Discomfort in the abdomen.
- Allergic Reactions: In rare cases, antibiotics can cause allergic reactions, such as rash, hives, or difficulty breathing.
9.4. Supportive Care: Relieving Symptoms at Home
In addition to antibiotics, supportive care can help relieve symptoms of strep throat. This includes:
- Rest: Getting plenty of rest to allow the body to recover.
- Fluids: Drinking plenty of fluids to stay hydrated.
- Warm Liquids: Soothing the throat with warm liquids such as tea or soup.
- Gargling with Salt Water: Reducing inflammation and relieving pain.
- Pain Relievers: Over-the-counter pain relievers such as acetaminophen or ibuprofen can help reduce fever and pain.
- Humidifier: Using a humidifier to keep the air moist and prevent the throat from drying out.
Outdoor activities are a great way to maintain a healthy family lifestyle during your travels.
10. Prevention Strategies for Families: Minimizing the Risk of Strep Throat
Preventing strep throat is crucial, especially for families who travel frequently. Implementing effective strategies can significantly reduce the risk of infection.
10.1. Good Hygiene Practices: Handwashing and Respiratory Etiquette
Good hygiene practices are fundamental in preventing the spread of strep throat. These include:
- Frequent Handwashing: Wash hands thoroughly with soap and water for at least 20 seconds, especially after coughing, sneezing, or being in public places.
- Use of Hand Sanitizer: When soap and water are not available, use hand sanitizer with at least 60% alcohol.
- Covering Mouth and Nose: When coughing or sneezing, cover the mouth and nose with a tissue or the elbow.
- Avoiding Touching Face: Avoid touching the face, particularly the mouth and nose, to prevent the transfer of bacteria.
10.2. Avoiding Close Contact with Infected Individuals
Minimizing close contact with individuals who have strep throat can help reduce the risk of infection. This includes:
- Staying Home When Sick: If a family member has strep throat, they should stay home from school or work to prevent spreading the infection.
- Avoiding Sharing Items: Do not share utensils, cups, or personal items with infected individuals.
- Maintaining Distance: Keep a safe distance from individuals who are coughing or sneezing.
10.3. Boosting the Immune System: Healthy Diet and Lifestyle
A strong immune system can help the body fight off infections, including strep throat. Ways to boost the immune system include:
- Healthy Diet: Eating a balanced diet rich in fruits, vegetables, and whole grains.
- Regular Exercise: Engaging in regular physical activity.
- Adequate Sleep: Getting enough sleep to allow the body to recover and repair itself.
- Stress Management: Managing stress through relaxation techniques such as yoga or meditation.
By incorporating these prevention strategies into your family’s routine, you can significantly reduce the risk of strep throat and ensure a healthier and more enjoyable travel experience.
Planning a family trip should be an exciting and stress-free experience. At familycircletravel.net, we provide comprehensive resources and tips to help you plan the perfect getaway. From destination ideas to travel safety advice, we’ve got you covered. Contact us today at 710 E Buena Vista Dr, Lake Buena Vista, FL 32830, United States, or call +1 (407) 824-4321. Visit our website familycircletravel.net for more information and to start planning your next adventure.
FAQ: Addressing Common Concerns About Strep Throat
1. How Long is Strep Throat Contagious?
Strep throat is contagious until 24 hours after starting antibiotics.
2. Can You Get Strep Throat More Than Once?
Yes, it is possible to get strep throat multiple times.
3. Is Strep Throat Always Accompanied by a Fever?
Not always, but fever is a common symptom.
4. Can Strep Throat Cause a Rash?
Yes, strep throat can cause a rash known as scarlet fever.
5. Can Adults Get Strep Throat?
Yes, adults can get strep throat, although it is more common in children.
6. How Accurate is the Rapid Strep Test?
The rapid strep test is generally accurate, but false negatives can occur.
7. What Should I Do If I Think My Child Has Strep Throat?
Consult a healthcare provider for diagnosis and treatment.
8. Can I Treat Strep Throat Without Antibiotics?
Antibiotics are necessary to treat strep throat and prevent complications.
9. What are the Symptoms of Strep Throat in Toddlers?
Symptoms in toddlers may include fever, irritability, and decreased appetite.
10. How Can I Prevent Strep Throat from Spreading in My Family?
Practice good hygiene, avoid close contact with infected individuals, and boost your immune system.